Adolescence is a high-risk period for the onset of mental disorders, and during this stage, mental illnesses have a more severe impact on individuals. High comorbidity, especially the coexistence of internalizing and externalizing mental disorders, is a significant characteristic of adolescent mental illnesses. Compared to individuals with a single type of mental disorder, those with comorbidity exhibit more severe cognitive and social functional decline, leading to a poorer prognosis. Current research often focuses on exploring imaging changes associated with single-type disorders, and there is limited attention to comorbidity and its imaging markers in adolescent mental disorders, hindering the understanding and effective treatment of the neural mechanisms underlying comorbid mental disorders.Does this comorbid condition simply imply a simple superposition of brain abnormalities related to a single disorder, or does it result in a qualitative change caused by quantitative variations, manifesting unique abnormal patterns different from those observed in various individual disorders?To answer this question, it is necessary to examine different structural modalities (such as cortical thickness and surface area) and investigate whether populations with single-type mental disorders (internalizing or externalizing) and comorbidities (both internalizing and externalizing) exhibit modality-specific patterns of changes, thus providing new insights into the neural mechanisms of comorbidity.
In recent years,the classification of psychiatric disorders into different diagnostic families using a dimensional approach has been recognized as a promising approach to address the high comorbidities, excessive diagnostic labels, and heterogeneity that currently exist in the diagnosis of psychiatric disorders.It serves as a method to address the issues of high comorbidity rates, excessive diagnostic labels, and heterogeneity in current psychiatric diagnoses. Adolescent mental disorders can be divided into two diagnostic families: externalizing disorders, representing cognitive/behavioral control issues, and internalizing disorders, representing emotional problems such as anxiety and depression.Typically, there are more comorbid patients within the same diagnostic family, leading to more research in these areas. However, limited research exists on comorbidity between different symptom spectra/diagnostic families.
On August 4, 2023 (USA local time), the research team led by Jie Zhang from the Institute of Science and Technology for Brain-inspired Intelligence at Fudan University, in collaboration with teams from McGill University in Canada and the University of Cambridge, published a research paper titled "Neurodevelopmental risk and adaptation as a model for comorbidity among internalizing and externalizing disorders: genomics and cell-specific expression enriched morphometric study" in the journal BMC Medicine. This study utilized multimodal imaging and genetic data from the international Adolescent Brain and Cognitive Development (ABCD) large-scale child imaging cohort and employed a mixed linear model to compare cortical surface area and thickness differences between externalizing disorders, internalizing disorders, comorbid externalizing and internalizing disorders, and a healthy control group. The study found that children with single-type disorders (either internalizing or externalizing) and those with comorbid internalizing and externalizing disorders exhibited specific patterns of changes in cortical surface area and thickness. Furthermore, the study revealed the association of these variation patterns with macroscopic behavioral and micro-scale genetic and cellular factors, providing evidence from neuroscience for the discovery of more sensitive imaging markers for comorbidity and a better understanding of the neural mechanisms of comorbid adolescent mental disorders.
Previous studies have indicated that cortical thickness and surface area are associated with psychopathological symptoms in adolescents and can serve as neuroimaging markers for adolescent mental disorders. However, current research is largely based on traditional diagnostic systems, focusing solely on individual mental disorders and single modalities, often with relatively small sample sizes. In this study, the research team utilized data from the Adolescent Brain Cognitive Development (ABCD) dataset, which includes baseline information from over 10,000 children aged 9-10 years across 22 sites in the United States. Employing a case-control analysis and a cross-diagnosis model, the team explored the patterns of cortical surface area and thickness changes in three groups of adolescents: those with externalizing disorders, internalizing disorders, and comorbid externalizing and internalizing conditions. Based on the identification of specific changes in cortical surface area and thickness, a comprehensive genome-wide association analysis (GWAS)was conducted to examine genetic loci associated with these measures. Subsequently, cell-specific analysis and enrichment analysis were performed to discover the cell types and enriched pathways related to variations in cortical surface area and thickness for both individual disorders and comorbid conditions (see Fig1)."
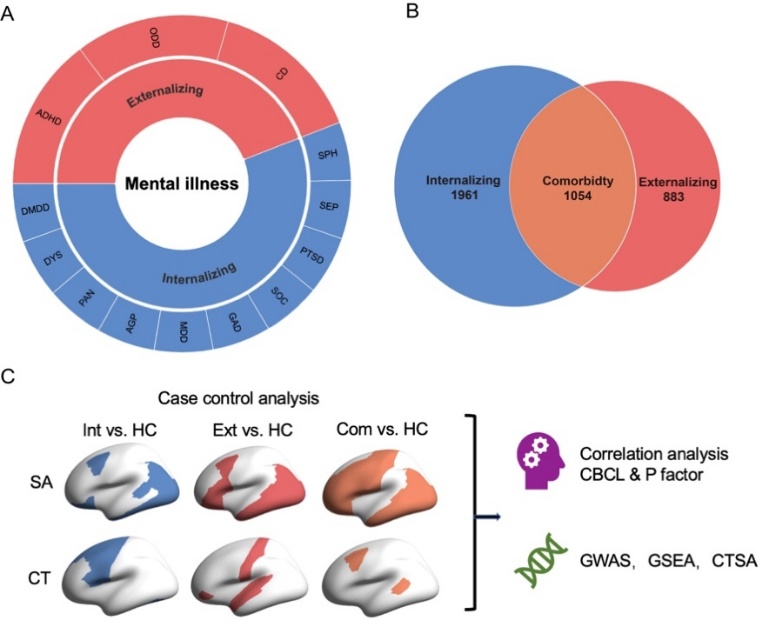
Fig1: analytical framework
Firstly, concerning the cortical surface area, compared to healthy children,those with comorbid disorders from different diagnostic families (externalizing and internalizing) exhibited significant reductions in cortical surface area throughout almost the entire brain, while children with single-diagnosis family disorders (either externalizing or internalizing) showed only a few brain regions with significant changes(see Fig 2, top row).
Secondly, regarding the cortical thickness, compared to healthy children,those with single-diagnosis family disorders displayed significant increases in cortical thickness (see Fig 2), while children with comorbid disorders from different diagnostic families did not show any brain regions with significant differences when compared to healthy individuals(see Fig 2, second row).
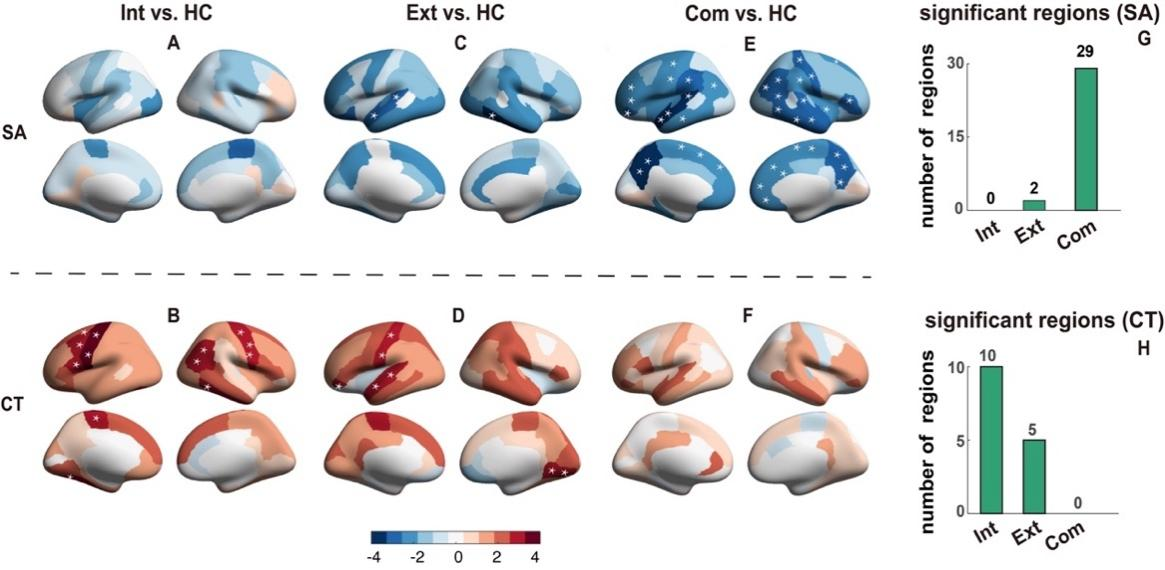
Fig2: Brain regions with significant changes in cortical areas when comparing externalizing disorders (Ext), internalizing disorders (Int), comorbid externalizing and internalizing disorders with healthy controls (HC). SA: cortical surface area; CT: cortical thickness
Third, in the comorbid group with cross-diagnosis, there was a significant reduction in cortical surface area in brain regions strongly correlated with externalizing symptoms (see Fig3). However, for children with single-diagnosis family disorders, brain regions with significantly increased cortical thickness did not show significant associations with the scores of psychopathological symptoms (see Fig4).
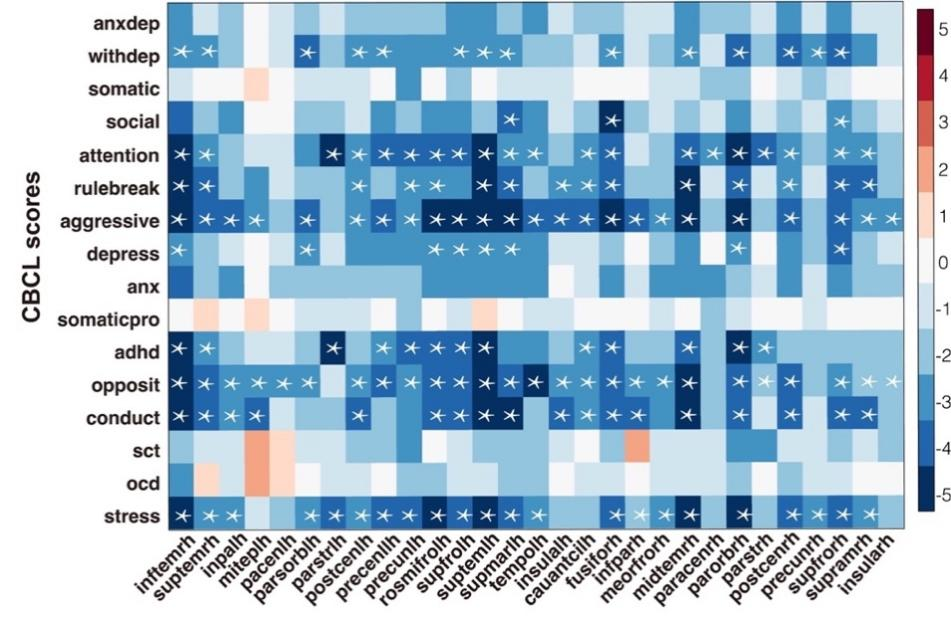
Fig3: Relationship between CBCL scores and significantly reduced cortical surface area in the brain
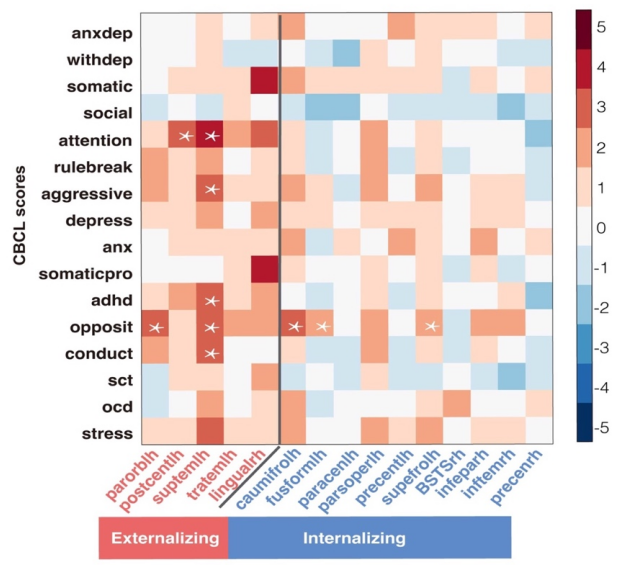
Fig 4: Relationship between CBCL scores and significantly increased cortical thickness in the brain
Fourth, the genetic analysis revealed distinct enriched pathways for cortical surface area and cortical thickness. The genes associated with cortical surface area enrichment were related to craniofacial microsomia and multiple system atrophy pathways, whereas the genes associated with cortical thickness enrichment were linked to immune-related pathways such as Immunoglobulin light chain amyloidosis.
Fifth, cell-specific analysis demonstrated that the cortical surface area and thickness features showing significant changes in the disease group were associated with different types of cells. The genetic pathways related to cortical surface area were specifically associated with inhibitory neurons, while the genetic pathways related to cortical thickness were specifically associated with astrocytes and oligodendrocytes.
According to the article, the lack of significant cortical thickness changes in individuals with comorbid cross-diagnostic conditions may be attributed to the opposing effects of two immune-related processes on cortical thickness: cortical pruning (associated with astrocytes) and myelination (associated with oligodendrocytes). These processes counteract each other, resulting in non-significant cortical thickness changes in the comorbid group.The study found that children with single-diagnosis family disorders and comorbid cross-diagnostic (externalizing and internalizing) conditions exhibited modality-specific imaging changes, indicating different sensitivities of distinct structural modalities to single disorders and comorbidity.Therefore, for clinical diagnosis of adolescent mental disorders, especially comorbid cross-diagnostic conditions, the choice of appropriate imaging modalities is essential. Additionally, the brain changes in adolescents with mental disorders may be regulated by various immune-related biological processes.
Dr. Nanyu Kuang from the Institute of Science and Technology for Brain-inspired Intelligence at Fudan University is the first author of this article. Researcher Zhaowen Liu from the School of Computer Science at Northwestern Polytechnical University, Dr. Chang Yu from The Chinese University of Hong Kong, and Postdoctoral Researcher Xinran Wu from the Institute of Science and Technology for Brain-inspired Intelligence at Fudan University are co-first authors. Professor Gunter Schumann from Fudan University, Professor Lena Palaniyappan from McGill University in Canada, and Researcher Jie Zhang from the Institute of Science and Technology for Brain-inspired Intelligence at Fudan University are the corresponding authors of the paper. This work was supported by the "Brain Science and Brain-like Research" major project of the Science and Technology Innovation 2030, the Shanghai Science and Technology Major Project on "Basic and Translational Research in Brain and Brain-like Intelligence," the National Natural Science Foundation of China, and the Key Laboratory of Computational Neuroscience and Brain-like Intelligence under the Ministry of Education.
OriginalArticle Link:https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-023-02920-9

