Recently, cooperating with researchers from University of Cambridge and King’s College London, professor Jianfeng Feng and Dr Qiang Luo’s research teams in the institute of science and technology for brain-inspired intelligence, Fudan University worked on the neural correlates of the dual pathway model for ADHD. They found gray matter volumes of the left cuneus were not only associated with the cognitive and motivational dysfunctions of ADHD, but also the genetic risk, and could predict ADHD symptoms 2 years later, which may serve as an imaging marker of ADHD. This study has been published in The American Journal of Psychiatry at May 7, entitled “Neural correlates of the dual pathway model for attention-deficit/hyperactivity disorder in adolescents”.
ADHD affects 5.9-7.1% children and adolescents worldwide, 50-66% of which persist into adulthood. In China, the prevalence of ADHD is about 6.3%. ADHD is characterized by inattention, hyperactivity and/or impulsivity. Past studies have reported high heterogeneity of the disorder, suggesting that there may be multiple independent pathways. The dual pathway model hypothesized two separable psychopathophysiological pathways leading to the symptoms of ADHD: cognitive dysfunctions such as deficits in working memory and attention regulation, and motivational dysfunction such as delay discounting. However, whether the hypothesized cognitive and motivational pathways had separable neural correlates is unclear.
Using a large European longitudinal neuroimaging cohort of adolescents (n=1963), researchers found lower gray matter volumes in prefrontal (e.g. left ventromedial prefrontal cortex, dorsal anterior cingulate cortex and anterior insular) and occipital (e.g. left cuneus) regions were associated with more severe ADHD symptoms (Figure 1).
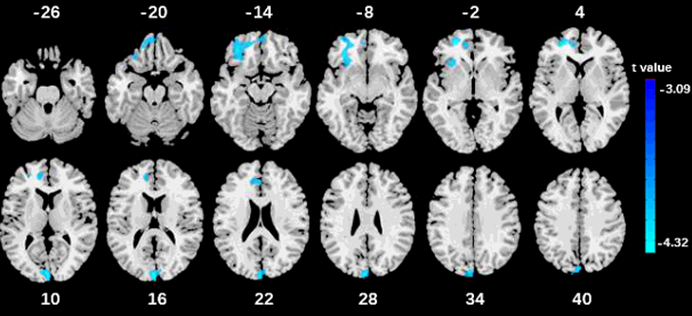
Figure 1: Lower gray matter volumes in prefrontal and occipital regions associated with more severe ADHD symptoms
Researchers further found gray matter volumes in the occipital region were negatively associated with working memory, attention regulation and delay discounting. In other words, the cognitive and motivational pathways have the shared correlate in the left cuneus. This finding may make an important revision to the dual pathway model especially the hypothesis of independent brain circuits.
Researchers found significant associations between the genetic risk of ADHD (i.e. polygenic risk score) and ADHD symptoms, working memory and delay discounting, and only the left cuneus in brain level. Dr Qiang Luo, one of the main researchers, said: “By longitudinal analysis, we also found gray matter volumes in the left cuneus at age of 14 could significantly improve the prediction accuracy of ADHD symptoms 2 years later.”
In an independent clinical dataset, never-medicated ADHD patients had the lowest gray matter volumes in these regions, the healthy controls had the highest, and the medicated patients had the intermediate gray matter volumes. Barbara Sahakian, the fellow of the British Academy and the Academy of Medical Sciences, distinguished professor of Fudan University, honorary doctorate of University of Cambridge, professor of department of psychiatry, commented : “Using large-scale neuroimaging data , this important study provides novel evidence that ADHD treatment medication does rescue the abnormally smaller volumes of key brain regions in patients with ADHD.”
In conclusion, this study suggests that the dual pathway model has both shared and separable neuroanatomical correlates. Especially, gray matter volumes in the left cuneus is associated with ADHD symptoms, both cognitive and motivational dysfunctions, the genetic risk and ADHD medication, and could predict ADHD symptoms 2 years later. Therefore, the left cuneus has a potential to serve as an imaging trait marker of ADHD.
According to professor Jianfeng Feng, the findings may help develop the imaging marker of ADHD, accurate diagnosis and efficacy evaluation.
Chun Shen, a PhD candidate in the institute of science and technology for brain-inspired intelligence, is the first author, and professor Jianfeng Feng and Dr Qiang Luo are the co-corresponding authors. This study is funded by the National Natural Science Foundation of China, the Key Project of Shanghai Science & Technology, Shanghai Municipal Science and Technology Major Project and so on.
ENDS
Paper available to view: https://ajp.psychiatryonline.org/doi/full/10.1176/appi.ajp.2020.19020183

